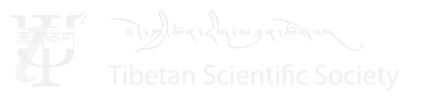
Big Bone disease, or rutim in Tibetan, is commonly known as Kashin-Beck disease (KBD). The disease affects the form and the mobility of the joints of the limbs, the growth and the length of the long bones at maturity and, in some cases, the global stature (Picture 1) [2]. To a common Tibetan villager, whose livelhood is primarily through manual work, having this progressive disease meant handicapped for whole life. Also, the occasional pain in the joints and bones in a resource crunch areas like remote villages in the Tibet was not less than a nightmare. Unfortunately, the survey found that the majority of KBD patient lived in the rural areas and were young.
-
Picture 1 Patient with Kashin Back Disease
From the year 1992 to 2002, Médecins Sans Frontières-Belgium (MSF) has launched different programs on KBD in TAR. The programs mainly focused on three aspects of KBD: curative health care and training, physical therapy study and epidemiological study. However, when MSF withdrew from TAR in the year 2002, same team of KBD researchers decided to continue the program and also initiate different programs under the name of the non-profit organization called Kashin-Beck Disease Fund (KBD-F).
The primary aim of this article is twofold –
- To pay tribute to all the researchers, led by MSF and KBD-F, who have been for so many years working on different causal hypothesis of KBD in TAR with one common goal i.e., to eradicate KBD from TAR.
- To create awareness among growing number of Tibetan researchers/students who have the required facility, talent and inclination to serve Tibetan inside Tibet.
For creating awareness, this article may serve as a short review on KBD research in TAR. If the reader wished to go deeper in the subject, one can consult the bibliography including a book reference [2] or few articles [3-12].
One among the first challenges the MSF network researchers faced in TAR was a lack of authentic and precise record on the number of people clinically affected by KBD. The reason for non-availability of authentic number of KBD patients in TAR was due to improper diagnosis of the disease. Hence, the first thing the researchers did was to develop new diagnostic protocol and thereby classify the KBD disease in three clinal stages [3]. The new diagnosis protocol involved use of more standardize tool like caliper (Picture 2) to measure joint deformities along with more subjective inference like inquiring the intensity of joint pain. Based on those diagnostic parameters, the patients were classified into three clinical stages of KBD. Once a proper diagnostic protocol was established, the researchers tested physical therapy study as curative and preventive treatment to alleviate pain, joint mobility, etc.

The physical therapy study [4] was conducted on 135 KBD patients, dividing them into two groups – study group (72 patients) and control group (63 patients). The study group were given physical therapy treatment twice a week and evaluated for pain and joint mobility after every five treatments. After about three years of physical therapy studies, the researchers observed that the treatment has improved range of joint mobility and pain at the beginning of study, however, the significant difference between the two groups decreased over the timeTherefore, the researchers had started to investigate the root cause(s) of KBD in TAR through series of epidemiological study.
In the first epidemiological study, researchers had found that the KBD children were iodine deficient. The barley grains stored at home were highly contaminated with 3 fungi. Also, the grains from KBD families were darker than those stored by non-KBD families, indicating a possible rule of the barley variety. They consumed water containing higher total organic content due to smaller container size and less time of decantation. It was also observed that the children from families with access to different nutrients were relatively protected from the disease. Based on these findings, a second epidemiological study was conducted through a prevention trial study to try to protect the children from the disease and to better understand the risk factors of the disease.
The following three hypotheses were tested in this study –
- Iodine, vitamins and minerals deficiencies
- Contamination in drinking water
- Fungal contamination in barley grains and tsampa (roasted flour made out of barley)
This prevention trial was conducted for about five years between the year 1998 and 2002 including 997 children aged between 5 to 15 years from 22 villages distributed over three prefectures (Lhasa, Shigatse and Lhoca). The study group were sub-grouped into five intervention categories to test the combination of the different hypotheses. At the end of the study, the prevention trial could only show that there is a significant improvement of some clinical indices in the antioxidant supplemented group as compared to the randomized placebo group that only received grain disinfection and iodine. Again, it was concluded that the clinical improvement in the study was consistently highest in the children with access to more diversified food. Hence, leading to third epidemiological study called clinical trial based on nutritional issues.

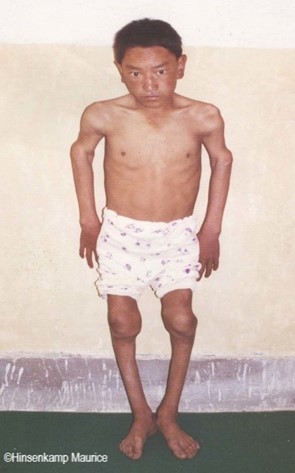
Good nutrition means combination of variety of nutrients. In this case, it is difficult to specify which nutrient is corelated directly with KBD or identified as a risk factor in TAR. Therefore, researchers analyzed urine and blood samples of people living in the KBD-endemic rural areas of South-Central Tibet to find any specific nutritional deficiencies. The study showed a very disturbing result that the population living in the KBD-endemic areas had series of severe nutritional deficiencies and/or imbalance. The report revealed that many children suffered from goiter suggesting an iodine deficiency, also rickets disease was prevalent, and vitamin A, vitamin E and very low concentrations of important trace elements were found deficient. Since it was difficult to correlate any one nutritional deficiency to the etiology of KBD in endemic area, the researchers had designed randomized clinical trial to evaluate the effect of a combined micro-nutrient supplementation (Picture 3) including all micro-nutrients known to be deficient in the population studied.

From the third epidemiological study, the researcher found that iodine supplementation for children with KBD is more effective than supplementing it with either selenium [5], calcium or vitamin D [6]. Although calcium and vitamin D supplementation failed to improve growth and bone metabolism of children living in a KBD-endemic rural area of Tibet, it improved their dental health. Interestingly, yet in some another studies [7, 8], researchers found that there were significant differences in mineral content between the endemic and the non-endemic area especially for wheat flour. In their monotonous diet, most of the children do not receive the Chinese dietary recommended intakes.
But since the very beginning of the research, it was also observed that there was difference in mycological contamination of barley grains stored in the KBD-endemic and KBD-non-endemic area and led to another study called the fungal hypothesis.
If the researcher could correlate to one KBD risk factor like certain fungi in the stored barley grains, it could be relatively easy to prevent KBD in rural Tibet. Therefore, very detailed investigation involving fungal analysis of barley, at different stages of barley to stored tsampa was initiated since the late nineties. Among many findings out of this study [9-12], interestingly, the mean percentage of grains contaminated with fungus called Alternaria was significantly higher in KBD-endemic area (29.6%) as compared to the KBD-non-endemic area (1.9%) in TAR. This let to further investigation and detection of erstwhile unknown mycotoxin produced by fungus Alternaria in stored barley from KBD-endemic area [12]. This gave strong correlation between fungal hypothesis and KBD in TAR.
With all the scientific research conducted so far, it was apparent that the etiology of KBD endemic in rural TAR was based on multiple contributing factors. Probably, at this stage, the curiosity driven research would have come to an end, more so when MSF withdrew from TAR after about 10 years and the researcher would have moved on to solve another problem. However, it was not the case here. The same group of researchers decided to continue the program and added some new program through newly formed non-profit organization called Kashin-Beck Disease Fund KBD-F).
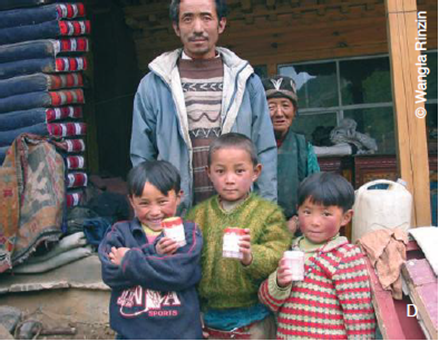
It is also heartening to see that researchers were not only interested in their scientific pursuit on KBD but also worked with local health providers to deploy many KBD preventive measures in different villages in TAR. The researchers had deployed health supplements to children, distributed posters to educate farmers (Picture 4) about importance of drying and storage of barley, helped to set up appropriate storerooms and containers for grains, distributed one device per village to measure grain humidity (Picture 5) before storage in order to curb fungal growth, biocide to disinfect seeds, built more than 1,600 family greenhouses to encourage food diversification, set up a KBD laboratory in Lhasa CDC and introduced sanitary program. There may be many other initiatives I might have missed but also a noteworthy one is program called PROTINET.
The objective of PROTINET (Program on Tibetan nettles) was to increase the interest of local Tibetan populations regarding their ancient knowledge and tradition of nettle consumption, as well as an establishment of nettle parcels in village. The researchers have also experimented on providing new nettle recipes to motivate children to increase their nettle intakes. They have also experimented with about 90 families on cultivating nettle gardens using different methods. Since nettles contain a variety of micronutrients, it could be a practical viable mean to reduce malnutrition among Tibetan children in the long run and thereby can potentially prevent other diseases.
Adhering to the Tibetan tradition, I would like to conclude this short article with a prayer. May all the researchers and health workers undertaking this compassionate work against KBD in general and TAR in particular receive all the required supports. May all KBD patients and villagers in TAR make progress towards right direction guided by education and awareness in order to curb disease such as KBD and alike. Long live MSF. Long live KBD-F.
For more information and resources on work being done on KBD in TAR, please visit http://www.kbdfund.org/books---symposium---publications.html
References
- Yardley J. Stunted by Illness, Tibetan Villagers ponder flight. The New York Times. September 29, 2003.
- Malaisse F, Mathieu F. Big Bone Disease, A multidisciplinary approach of Kashin-Beck disease in Tibet Autonomous Region. 2008. ISBN 978-2-87016-093-0.
- Mathieu F, Begaux F, Lan Z, Suetens C, Hinsenkamp M. Clinical manifestations of Kashin-Beck disease in Nyemo Valley, Tibet.Int Orthop. 1997;21(3):151-6
- Mathieu F, Suetens C, begaux F, De Martelaer V, Hinsenkamp M. Effects of physical therapy on patients with Kashin-Beck disease in Tibet. Int Orthop. 2001;25(3):191-3.
- Moreno-Reyes R, Mathieu F, Boelaert M, Begaux F, Suetens C, Rivera MT, Neve J, Perlmutter N, Vanderpas J. Selenium and iodine supplementation of rural Tibetan children affected by Kashin-Beck osteoarthropathy. Am. J. Clin. Nutr. 2003, 78:137–144.
- Rooze S, Mathieu F, Claus W, Yangzom T, Yangzom D, Goyens P, De Maertelaer V. Effect of calcium and vitamin D on growth, rickets and Kashin–Beck disease in 0- to 5-year-old children in a rural area of central Tibet. Trop. Med. Int. Health. 2016, 21: 768-775.
- Dermience M, Mathieu F, Barthélemy J.-P, Maesen Ph, Romnee J.-M, De Maertelaer V, Yangzom D, Tsewang P, Lognay G. The relevance of food composition data for nutrition surveys in rural Tibet: pilot study in the context of Kashin-Beck Disease. Biotechnol. Agron. Soc. Environ. 2013, 17: 32-42.
- Dermience M, Mathieu F, Li X.W, Vandevijvere S, Claus W, De Maertelaer V, Dufourny G, Li Bin, Yangzom D, Lognay G. Minerals and Trace Elements Intakes and Food Consumption Patterns of Young Children Living in Rural Areas of Tibet Autonomous Region,
R. China: A Cross-Sectional Survey. Healthcare 2017, 5 - 12. - Chasseur C, Suetens C, Nolard N, Begaux F, Haubruge E. Fungal contamination in barley and Kashin-Beck disease in Tibet. Lancet. 1997, 350: 1074.
- Chasseur C, Suetens C, Michel V, Mathieu F, Begaux F, Nolard N, Haubruge E. A 4 year study of the mycological aspects of Kashin-Beck disease in Tibet. Int. Orthop., 2001, 25: 154-158.
- Haubruge E, Chasseur C, Suetens C, Mathieu F. Begaux F, Malaisse F. Mycotoxins in Stored Barley (Hordeum vulgare) in Tibet Autonomous Region (People’s Republic of China). Mountain Research and Development. 2003, 23: 284–287.
- Haubruge E, Chasseur C, Debouck C, Begaux F, Suetens C, Mathieu F, Michel V, Gaspar C, Rooze M, Hinsenkamp M, Gillet P, Nolard N, Lognay G. The prevalence of mycotoxins in Kashin-Beck disease. Intern. Orthop., 2001, 25: 159-161.